IFCDC- Recommendations for Skin-to-Skin Contact with Intimate Family Members
"Imagine....feeling frightened at the thought of holding your baby.... then turning the fear into confidence when your nurse guides you to do skin-to-skin care with your baby. I loved this time with my daughter; she always seemed so peaceful sleeping on me.”*
These committee members had primary responsibility for this section:
Raylene Phillips, MD, MA, FABM, FAAP, IBCLC
Karen Smith, MEd, RNC
Questions to consider when starting your process Skin To Skin Contact With Intimate Family Members
Check sheet to assess this area before and after intervention.
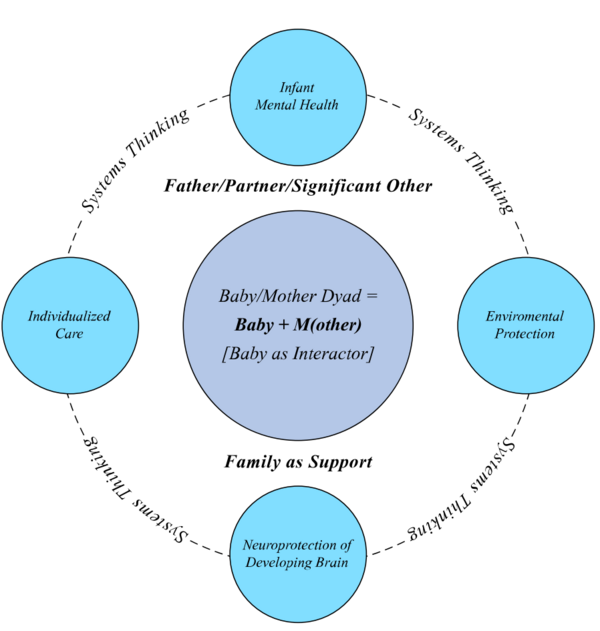
Successful change only happens in relation to the system. To review systems concepts check this section.
Standard 1, Skin-to-Skin Contact: Parents shall be encouraged and supported in early, frequent, and prolonged skin-to-skin contact (SSC) with their babies.
Competency 1.1: Verbal and written information about the benefits of SSC shall be provided to parents (including fathers) in their primary language whenever possible and as early as possible before or after intensive care unit (ICU) admission.
Competency 1.2: Information in a variety of appropriate formats and in the parents’ language should be provided about the SSC policy and how it applies specifically to them and their baby including: a) inclusion and exclusion criteria; b) indications and techniques for kangaroo care (KC) and hand containment (HC); and c) who may be designated by parents to participate in SSC.
Competency 1.3: Images of individuals from diverse populations doing KC and HC should be placed in prominent locations in the hospital and ICU.
Competency 1.4: Parents should be given opportunities to practice SSC transfer with an appropriately-sized manikin if desired before transferring their own baby.
Competency 1.5: Parents should be provided with comfort including: a) safe and comfortable seating or reclining accommodations that are readily available at baby's bedside; b) support pillows; c) secure wraps to support baby; d) a mirror to see baby’s face; e) hydration and nutrition for parents as needed; f) privacy, if desired (in private rooms or by privacy screens); and g) a quiet, therapeutic environment for being with their baby.
Competency 1.6: A healing environment that protects the baby's physiologic and behavioral stability shall be maintained during SSC including: a) appropriate room temperature with absence of drafts; b) consistently low sound levels; c) avoidance of bright lights with individualized light as needed to assess baby; d) prominence of parent’s scent (free of strong scents including perfumes and tobacco); e) proximity to mother’s breast to support smell and taste (when a mother providing milk is holding her baby); and f) gentle touch and handling to protect baby’s immature vestibular system.
Competency 1.7: Parents shall be supported to recognize their baby's behavioral communications of stress and relaxation during SSC.
Competency 1.8: Parents shall be encouraged to support their baby in SSC during painful procedures whenever possible.
Competency 1.9: Parents shall be encouraged to have vocal and singing interactions with their baby during SSC to enhance parental-infant connections, reduce parental anxiety, increase newborn vocal/listening interactions, and improve the baby’s autonomic stability.
Competency 1.10: Parents should be allowed to fall asleep during SSC or Kangaroo Care (KC) when safety measures are in place that include: a) parent and baby are in a non-rocking, reclining chair or bed; b) baby is well secured by an appropriate wrap to parent's chest; c) baby is electronically monitored, if indicated; and d) an appropriate healthcare provider is immediately available.
Evidence-Based Rationale:
Parents need information to appreciate the therapeutic effects of SSC with their baby in the ICU and deserve information that is clear and understandable, free from medical jargon, and in their native language. (2, 3) A pre-selected teaching DVD on SSC may be useful for parents to watch before doing SSC of very premature or sick babies. Fathers often need specific encouragement to hold their baby in SSC, and should be included in all educational efforts and SSC opportunities. (4, 5) Parents need to see role models within their own culture and ethnicity doing KC and HC. (6, 7)
Parents should be invited and encouraged to have early, frequent and prolonged SSC with their baby whenever possible. Parents are often intimidated by the ICU environment and by the size and medical condition of their baby and may need reassurance, support, and encouragement to engage with their baby in the ICU. (8, 9) SSC/KC has been shown to reduce maternal anxiety in the NICU. (10) Parents may need instructions on developmentally appropriate HC, and they may wish to practice a simulation of KC with a manikin before doing it with their baby. Supporting parents in how to recognize their baby’s behaviors communicating stress and relaxation help to reduce maternal stress. (11) Supporting parents in having SSC with their baby reinforces their role as a parent and as an active member of the caregiving team. (12) Many parents want to be involved in comforting their baby during painful procedures, and should understand how and why SSC can give them an opportunity to do so.(13-15)
Safety and comfort are essential if frequent and prolonged SSC is to be achieved. (16) Comfortable seating or reclining accommodations, including adult beds or reclining chairs whenever possible (non-rocking for intubated babies), should be available to facilitate SSC whenever parents are present. Mothers may need extra support to be comfortable for days/weeks after giving birth. The use of wraps to secure babies in the KC position has been shown to provide comfort, safety, and encourage more SSC. (17) Breastfeeding mothers need hydration and nutrition on a regular basis. Babies who are being electronically monitored should continue monitoring during KC, and should also be visually monitored by a healthcare provider when the parent is asleep during SSC.
Many m/others (and sometimes fathers) desire privacy during transfer when their chest is exposed, and during SSC for enhanced bonding with their baby. Parents often need support in just being a parent, and understanding that their baby’s behavioral communications can help create an emotional connection with their baby in the ICU. (18, 19) Because it is sometimes difficult to see baby's face during KC, a mirror can provide another means for parents to connect with their baby. Utilizing Kangaroo Supported Diagonal Flexion (KSDF) positioning provides more opportunities for mother–baby eye-to-eye contact, maternal vocalizations, smiles, and caressing. (20) Parental talking and singing during SSC can reduce anxiety and improve autonomic stability in stable preterm babies. (21) Babies born prematurely, who spend their first weeks and even months of life in the ICU, are often exposed to excessive levels of sound. If separated from mother, they are deprived of the maternal sounds they would otherwise hear in utero. Evidence suggests that the functional development of the auditory system is largely influenced by environmental acoustic inputs early in life, and hearing m/other’s voice enhances hearing development and physiological stability. (22, 23)
While thermal synchrony with the parent will usually keep baby warm, some rooms have extreme temperatures that should be noted, and accommodation made. (24) SSC stimulates oxytocin and neuropeptide release promoting localized vasodilation, and increased skin temperature of the mother’s breast tissue, thus promoting newborn thermoregulation. Loud sounds are destabilizing to premature and sick babies, and can interrupt sleep. (25) ICU staff conversations and monitor alarms are the primary sources of loud noise levels in the ICU. In addition, direct light can interfere with sleep and strong scents can be destabilizing to premature and sick babies. (25) Babies are known to recognize and prefer mother’s scent (26). The early smell and taste of mother’s milk provides positive oral and gustatory experiences. It is important to recognize that all handling of the baby should be done slowly so as not to overstimulate the baby’s immature vestibular system. (27, 28)
Having a baby in the ICU is mentally, emotionally, and physically exhausting, and parents are usually chronically tired. (29) If safety measures are in place, prolonged SSC in KC is a good intervention for both baby and parent to promote rest and sleep. In addition to secure positioning and electronic monitoring (if indicated), an appropriately trained healthcare provider must be immediately present whenever a parent is asleep during KC.
Standard 2, Skin-to-Skin Contact: Education and policies in support of skin-to-skin contact between parents and their baby shall be developed, implemented, monitored and evaluated by an interprofessional collaborative team.
Competency 2.1: A written policy and education/training plan for SSC shall be: a) known by all ICU interprofessional staff; b) reviewed by all new employees during employee orientation and annually; and c) evaluated every 1-3 years by ICU leadership for any needed updates.
Competency 2.2: The SSC policy shall include: a) strategies for keeping the baby together with m/other as much as possible; b) clear inclusion and exclusion criteria for SSC; and c) who may be designated by parents to participate in SSC.
Competency 2.3: SSC staff education plan shall include didactic education about: a) the developmental and physiologic expectation of all newborn babies to be in continuous SSC contact with their mothers after birth and the stress induced by separation; b) the multiple benefits of SSC for babies including decreased mortality, improved physiologic stability, reduced stress and pain, optimal sleep, enhanced neurodevelopment, enhanced gut microbiome maturity, improved feeding tolerance, increased growth, early initiation and longer durations of breastfeeding, decreased rates of sepsis, enhanced parental-infant attachment and bonding; c) the benefits of SSC for parents including reduced stress and anxiety, enhanced parental-infant attachment and bonding, and increased breast milk production for mothers; and d) the need for a healing environment during SSC including protection from loud sounds, bright lights, and strong scents and practical ways to create and maintain such an environment. (White, 2013)
Competency 2.4: SSC staff training should include simulation training with appropriately-sized baby manikin/doll on how to safely do standing and sitting transfers of baby (including babies on mechanical ventilation and with lines) to parent’s chest.
Competency 2.5: ICU staff who are experienced and comfortable with SSC transfers should be available to mentor less experienced staff until they gain competence and confidence in facilitating SSC transfers.
Competency 2.6: SSC educational content should include ways to individualize SSC according to the baby’s medical condition, behavior and state organization and should include: a) descriptions, techniques and indications for KC or gentle supportive HC; and b) techniques and scripts for supporting use of these options to parents.
Evidence-Based Rationale:
Formal policies legitimize care practices as standards of care, and help to standardize practice methods. (31) Policies that are fundamental to the culture of the unit need to be introduced early, during orientation after employment begins. A SSC policy should clearly describe the inclusion and exclusion criteria for SSC/KC, and define who may participate in SSC/KC to avoid ambiguity and confusion. Staff education should explain that maternal proximity is the developmental and physiological expectation of all newborn mammals and the "natural habitat" for all newborn altricial mammals. (32) Education should include evidence in neuroscience and neurobiology that supports the importance of SSC on newborn brain development (33). Much research (animal and human) documents the universal stress reactions experienced by both mothers and babies when they are separated; (34, 35) therefore, barring extreme medical circumstances, every effort should be made to keep babies with m/other as much as possible for optimal physiologic stability and neurodevelopment.
SSC is one of the most studied interventions in neonatal care. The benefits of SSC documented in numerous studies include: decreased mortality, (36, 37) improved physiologic stability, (38) reduced stress and pain, (13-15) optimal sleep, (39) enhanced neurodevelopment, (33, 40, 41) enhanced gut microbiome maturity, (42) improved feeding tolerance, (43) increased growth (44, 45), early initiation and longer durations of breastfeeding, (37, 46, 47) decreased rates of sepsis, (36, 46) reduced parental stress and anxiety, (14) and enhanced parental-infant attachment and bonding. (14, 36, 41, 48-50) In addition, SSC increases maternal, paternal and infant oxytocin levels, which support bonding and attachment and increases prolactin levels in mothers, which increases milk production. (14, 51, 52)
Since staff are responsible for creating and maintaining a healing environment in the ICU, they need information about the importance of individualizing light, sounds, and scents in ways that will protect babies in the ICU from developmentally inappropriate stimulation. In addition to knowledge of the rationale, staff need practical methods of applying this knowledge to support parents and babies during SSC. Staff need more than knowledge and theory to enthusiastically support SSC. Simulation training provides practical, hands-on experience during the learning process to develop competency and confidence in new skills and can be done with appropriately-sized baby/doll manikins to demonstrate how to safely perform standing and sitting transfers of babies (including intubated babies) to parent’s chests (53). Many studies have documented the safety of SSC/KC with ventilated babies, (54, 55) and at least one prospective study with 263 VLBW babies has documented the safety of SSC with umbilical lines (56). A support team for both day and night shifts can provide ongoing assistance, which is often needed during the early stages of practice with a new skill.
All care, including SSC, should be provided in a manner individualized to the baby's developmental stage and adapted to age, medical condition, stability, and state availability. (27, 28) While KC is usually the first choice for SSC, if it is contra-indicated, parents should be encouraged to provide developmentally appropriate HC for their baby. Providing KC or HC for a tiny, fragile baby can be frightening to parents and they may need reassurance and a demonstration of techniques.
Standard 3, Skin-to-Skin Contact: Babies shall be evaluated to: a) determine their readiness for transfer to KC; b) assess stability during transfer from bed to parent's chest; c) assess baby's response to SSC (KC or HC); and d) assess their stability during and after transfer back to the bed.
Competency 3.1: A standardized assessment of the baby's readiness, stability and response to transfer and to SSC should be utilized by ICU staff.
Competency 3.2: Electronic or manual documentation should be created, and staff should be trained in methods of entering data to record parameters, such as: a) if baby was eligible for KC, b) if KC and/or HC was offered to parent; c) if KC or HC was done and how long; d) which parent had SSC with baby; e) baby’s response; f) parent’s experience; and g) staff experience/motivation.
Competency 3.3: Periodic quality improvement (QI) evaluations should be conducted using validated methodology to evaluate SSC implementation and sustainability.
Evidence-Based Rationale:
Standardized evaluation and documentation will aid in monitoring safety and therapeutic value in SSC. A variety of valid assessments for SSC are available. (16) Accurate and consistent data collection will make it possible to evaluate progress and identify quality improvement opportunities. Without formal plans for a QI process, it is unlikely to occur. Participation in formal QI processes with other institutions provides comparison of progress and motivation for improvements. (58, 59)
Standard 4, Skin-to -Skin Contact: Parents shall be provided information about the benefits of SSC that continue for babies and parents after discharge.
Competency 4.1: Discharge planning with parents shall include information regarding the continued value of SSC, holding of babies, and encouragement for parents to continue SSC at home.
Competency 4.2: Parents shall be supported in how to safely hold and carry their baby after discharge, including the use of a baby carrier if desired.
Evidence-Based Rationale:
The benefits of SSC for babies and parents continues for several months after birth and has been shown to enhance neurodevelopment and social engagement, (50, 60) increase breastfeeding duration, (61) and reduce incidence of postpartum depression. (60) Safety is an ongoing issue that continues after discharge, so should be discussed with parents during discharge planning.
*Acknowledgement of Diane Maroney for consenting to our use of the concept of “imagine…” statements written by parents/families who have experienced intensive care; and to our parents for their thoughts.