IFCDC- Recommendations for Best Practice Reducing & Managing Pain & Stress in Newborns & Families
“Imagine…sitting by an isolette and begging and pleading with God for a miracle and mercy, and never really knowing if that is what’s best for your baby.”*
These committee members had primary responsibility for this section:
Michael T. Hynan, PhD
Robert Cicco, MD
Becky Hatfield
Questions to consider when starting your process Reducing And Managing Pain And Stress In Newborns And Families
Check sheet for babies and families to assess this area before and after intervention.
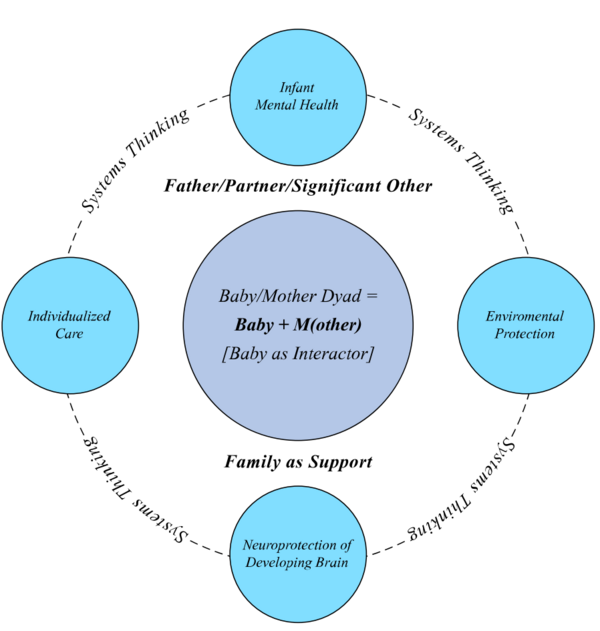
Successful change only happens in relation to the system. To review systems concepts check this section.
Standard 1, Pain and Stress, Families: The interprofessional team shall document increased parental/caregiver well-being and decreased emotional distress (WB/D) during the intensive care hospital (ICU) stay. Distress levels of baby’s siblings and extended family should also be considered.
Competency 1.1: Parents shall have unlimited opportunities to be with their baby and be encouraged to engage with their baby, including skin-to-skin interactions.
Competency 1.2: Education shall be provided to all parents on how to (a) recognize their baby’s behavioral communications of pain and distress as well as signs of comfort and (b) support parents to use practical ways to safely comfort and soothe their baby.
Competency 1.3: WB/D shall be evaluated within 72 hours of admission and 48 hours before discharge (as well as other times indicated by clinical judgment).
Competency 1.4: Training should be provided for staff in how to screen, assess and document parent/family WB/D in accord with ICU policies.
Competency 1.5: Evaluations of WB/D shall include informal and routine bedside conversations with all parent/caregivers by social workers and psychologists (one per 20 beds), who may utilize appropriate questionnaires and/or inventories to assess for postpartum depression (PPD), Post-Traumatic Stress Disorders (PTSD) or other mental health concerns. This information shall be communicated to relevant members of the interprofessional team in accord with ICU policies.
Competency 1.6: Standardized education programs on reduction of distress and anxiety in families shall be provided for all professionals and include topics: (a) provision of Infant and Family Centered Developmental Care; (b) recognition of symptoms of anxiety, PPD, and PTSD; (c) use of reflective listening skills and non-judgmental feedback; (d) understanding of implicit cultural biases; and (e) utilization of emotional and physical self-care.
Competency 1.7: All parent/caregivers shall be provided with psychoeducational groups emphasizing developmental care as well as the opportunity for peer-to-peer individual support by trained volunteers in the ICU.
Competency 1.8: Selected ICU staff should be appointed to provide targeted levels of support (e.g., listening visits) for parents/caregivers deemed at risk for emotional distress.
Competency 1.9: Appropriate emotional interventions and support shall be provided by social workers, psychologists, and psychiatrists within the ICU to parents/caregivers with debilitating levels of symptoms or acute distress.
Competency 1.10: Referrals of ICU family members for psychotherapy outside the ICU shall be provided using established hospital resources and referral strategies.
Competency 1.11: Discharge planning should include information about parent WB/D and related interventions. This information should be communicated to follow-up providers to promote optimal IFCDC at home.
Evidence-based rationale:
In general, prolonged and involved contact with babies, including skin-to-skin care has been shown to reduce parental distress. (1-5) Reports of elevated posttraumatic stress symptoms in NICU parents, with 60% of mothers and 47% of fathers scoring above threshold, came from an NICU that restricted parental presence to 6 hours in the afternoon, one at a time for parental contact, and did not permit skin-to-skin care or breastfeeding. (6) Global studies have documented increased risk of ICU mothers and fathers for perinatal mood disorders (PMDs). (7-10) These studies have uniformly recommended screening for PMDs in the ICU for the benefit of parents, the physical and emotional development of the baby, and family functioning. (11) Identification of those parents/caregivers who need intervention is necessary soon after the baby is admitted to the NICU and as the hospitalization progresses. (12-14) Formal and validated assessments and screeners are available to determine levels and trajectories of emotional distress, which may increase or decrease over time. (15-18) The benefits of universal care (19) for all ICU parents using peer-to-peer support and psychoeducation regarding developmental care principles have been documented. (20-22) Provision of targeted support for mothers has been well-received by NICU nurses and is associated with reduced depression in NICU mothers. (23, 24) A growing number of studies report improved outcomes for mothers who have received psychotherapy in the NICU. (25-27) Not all ICUs have the resources to provide therapy in the unit by mental health professionals. Professional responsibilities necessitate referral of these parents elsewhere.
Standard 2, Pain and Stress, Babies: The interprofessional collaborative team shall develop care practices that prioritize multiple methods to optimize baby outcomes by minimizing the impact of stressful and painful stimuli.
Competency 2.1: Standardized education centered on reduction of pain and stress in babies shall be provided to all interprofessional staff including physicians, NNPs and all newly hired professionals on a regular basis no less frequent than annually.
Competency 2.2: Educational offerings shall include the use of standardized pain assessment tools, recognition of the baby’s behavioral communication during stressful or potentially painful procedures, the value of skin-to-skin care in reducing stress, and the appropriate use of pharmacologic and non-pharmacologic interventions.
Competency 2.3: Assessment of pain and/or stress using a validated instrument shall be routinely and regularly administered and documented for all babies.
Competency 2.4: Opportunities for positive interactions with the baby’s parents and other caregivers, in particular with familiar loved ones should be prioritized.
Competency 2.5: Opportunities for closeness/skin-to-skin care, as appropriate, and family access to their baby at all times, including during procedures, shall be encouraged, documented and routinely evaluated.
Competency 2.6: Use of non-pharmacologic interventions such as positioning, non-nutritive sucking and appropriate swaddling shall be implemented according to the behavioral communication of the baby, documented and evaluated during routine care protocols within the ICU.
Competency 2.7: Pharmacologic interventions, including the use of sucrose and non-opioids, shall be reserved primarily for episodic painful or stressful procedural events, including retinal exams, intubations, post-operative pain management, etc. Their use shall be balanced against potential negative side effects.
Competency 2.8: When pharmacological therapy is utilized, non-pharmacologic interventions shall be used in conjunction with it as a component of a comprehensive pain and stress management strategy.
Competency 2.9: Pain and stress management should be individualized and based on each baby’s behavioral and physiological communication and consideration of the parents’ expressed preferences.
Competency 2.10: Appropriate information regarding pharmacological and non-pharmacological pain management options for their baby should be provided to parents; Parents shall be included in discussions and encouraged to participate in decisions about pain management for their baby.
Competency 2.11: Families should be included in the development of protocols for assessment and management of neonatal pain/stress, and these protocols shall be readily available to the interprofessional staff.
Evidence Based Rationale:
An abundance of data exists to provide documentation that babies, both term and preterm, experience pain and have both behavioral and physiologic responses to pain. (28-31) Furthermore, studies have also indicated that babies may recall painful stimuli weeks, months, or years after their occurrence with modified behavioral responses. (32-34) Despite this knowledge, assessments of pain and the use of pharmacologic and non-pharmacologic interventions vary greatly among NICUs. (30, 35) Non-pharmacologic interventions, including skin-to-skin care, have been shown to be effective in reducing both physiologic and behavioral signs of pain and stress. (36-39) Parents are uniquely qualified to participate in these non-pharmacologic interventions. They are especially sensitive to their baby’s behavioral communication and therefore most capable of providing positive sensory interactions that will modify the pain response and promote optimal brain development. (2, 40-42) Yet parents are often excluded from involvement during painful or stressful interventions when their inclusion can provide input that offsets painful or stressful interventions. Utilizing non-pharmacologic interventions as part of routine care will reduce the need for pharmacologic therapy for control of neonatal pain and stress. (39, 43-45) There is, however, a place for pharmacologic treatment (including sucrose and topical agents) for episodic procedural pain, including intubations and retinal exams and after surgeries. (46-48) Pharmacologic treatment will be more effective when used to complement non-pharmacologic interventions. There is insufficient evidence to recommend routine continuous pharmacologic treatment for mechanically ventilated newborns. (49) Furthermore, there are data to suggest that long term, or continuous use of some pharmacologic therapies, may increase the risk of adverse neurologic events, and lead to longer periods of mechanical ventilation. (50-52)
To provide maximum control of pain and stress in babies, treatments should be tailored to a baby’s individual signs and responses to interventions. (41, 53) Here again, parents are integral partners in making these observations and will be more effective partners when made fully aware of treatment options. Consistency in providing this individualized care will be enhanced by the development of standardized protocols that can be utilized by all caretakers. (41, 54) This will minimize variation in care of both staff members and parents in responding to a baby’s signs of pain or stress.
*Acknowledgement of Diane Maroney for consenting to our use of the concept of “imagine…” statements written by parents/families who have experienced intensive care; and to our parents for their thoughts.