IFCDC- Recommendation for Best Practices in Systems Thinking
“The biggest challenge is ‘medical professionals’ treating parents as though they are anxious beings who can’t handle information. If doctors, therapists, and nurses actually took the time to hear what parents are saying, then real problems could be identified early…” (1) (p.63)
These committee members had primary responsibility for this section:
Carole Kenner, PhD, RN, FAAN, FNAP, ANEF
Carol B. Jaeger, DNP, RN, NNP-BC
Questions to consider when starting your process Systems Thinking In Complex Adaptive Systems
Check sheet to assess this area before and after intervention.
The Committee has provided a list of questions to help ascertain your unit's current status on issues concerning the developmental care standards. Considerations for Implementation
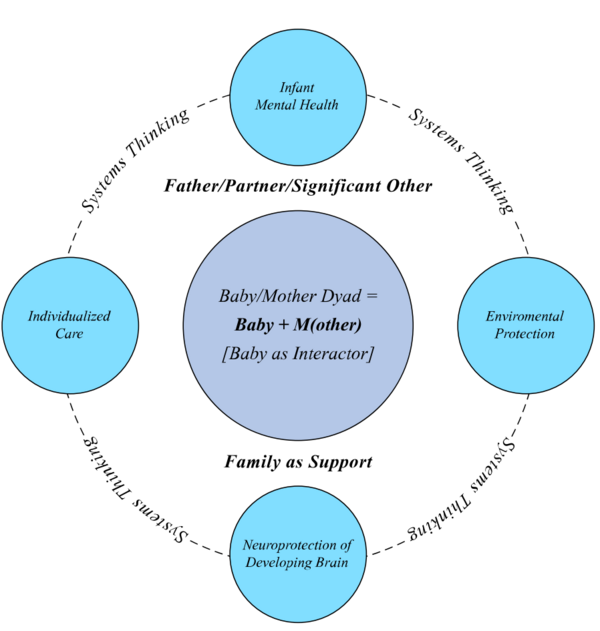
Standard 1, Systems Thinking: The intensive care unit shall exhibit an infrastructure of leadership, mission, and a governance framework to guide the performance of the collaborative practice of IFCDC.
Competency 1.1: An organizational vision, values, and goals for baby, parent, and family centered care in practice shall be articulated in verbal and written form, and be visibly represented in the unit.
Competency 1.2: With support to/from ICU parents and families, policies, procedures, education programs, interdepartmental relationships, culture, infrastructure, and physical and environmental design to optimize the baby’s physical and psychosocial development shall be identified.
Competency 1.3: Strategic policy(ies) of the governance framework, interprofessional role descriptions, and performance competencies consistent with IFCDC principles shall be developed, implemented and periodically evaluated.
Competency 1.4: ICU leadership will identify the process, indicator(s), evaluation expectation(s), and oversight of operational process and interprofessional IFCDC performance.
Competency 1.5: Appropriate evidence, regulation, education, and incentives to guide stakeholders to/through strategic initiatives will be monitored and regularly evaluated.
Competency 1.6: Leadership will demonstrate accountability to achieve the unit’s strategic improvement goals of organization and collaborative practice.
Evidence-based rationale:
Health organizations (macro, meso, and micro) are complex and dynamic—continuously changing and adapting. Administering and managing a complex system requires planning to define and develop the organizational vision, values, IFCDC, goals, infrastructure, role descriptions, policies, procedures, and process for the implementation of continuing change. The role of professional leaders is to provide direction and oversight by strategically managing change situation-by-situation amid the activities of daily operations, while simultaneously guiding individuals and teams to the "big picture" vision of a collaborative interprofessional practice that integrates evidence-based developmental family centered standards and principles. (2-14)
Standard 2, Systems Thinking: The intensive care unit shall provide a professionally competent interprofessional collaborative practice team to support the baby, parent, and family’s holistic physical, developmental, and psychosocial needs from birth through the transition of hospital discharge-to-home and assure continuity to follow-up care.
Competency 2.1: Teams will demonstrate IFCDC through interaction, practice implementation, and documentation that they are baby, parent, and family centered.
Competency 2.2: Teams will demonstrate interprofessional activities that bridge with community and neonatal population oriented services, such as ICU follow up clinics and community intervention programs.
Competency 2.3: The building of positive relationships among parents, family, and team members shall be demonstrated, and regularly evaluated.
Competency 2.4: Team activities, policies, and implementation of developmental and family centered care will demonstrate processes that support IFCDC.
Competency 2.5: Links to adult learning activities, educational strategies, and behavioral assessments should be identified and readily available to team members.
Competency 2.6: Participation in educational programs and team assignments shall demonstrate continued learning, and foster growth as an interprofessional team member.
Competency 2.7: Team members shall demonstrate systems context sensitivity applicable across practice settings and show respect for individual and collective professional skill sets (transprofessional).
Competency 2.8: Open and ongoing communication among team members including parents and families shall be encouraged.
Competency 2.9: Teams will manage real and potential conflict by using an adopted defined process to negotiate an effective resolution.
Competency 2.10: Interventions, education, and communication will use common and meaningful language across professions, and among professionals, parent(s), and family.
Competency 2.11: Respect for and integration of diversity and ethnic backgrounds shall be prioritized in policy development and practices.
Competency 2.12: All activities, educational programs and policies will be physical and social/emotional health outcome driven.
Evidence-based rationale:
Frenk and colleagues (15) state that education for health professionals in the 21st century must promote “interprofessional and transprofessional education that breaks down professional silos while enhancing collaborative and non-hierarchical relationships in effective teams.” (p1951) The health workforce must build a shared foundation of communication, collaboration, and interaction to effectively and efficiently access, plan, implement, and evaluate the provision of care to each baby and the baby’s family. The team members, inclusive of parents/family, recognize the role of each member and the significance of their effect on the complex system, as well as the system’s effect on the performance of the team engaging with babies and families for a better outcome. (12, 16-31)
Standard 3, Systems Thinking: The practice of IFCDC in the intensive care unit shall be based on evidence that is ethical, safe, timely, quality-driven, efficient, equitable, and cost-effective.
Competency 3.1: The ICU physical space, environment, and culture should be supportive of the health, wellbeing, and development of the baby and family.
Competency 3.2: Efforts to engage and integrate the family and interprofessional team in neonatal health continuing education; and the planning, implementation, and evaluation of improvement initiatives should be demonstrated, documented, and evaluated.
Competency 3.3: Regular assessment and evaluation of the level of competence, satisfaction and wellbeing experienced by both parents and health professionals should be implemented.
Competency 3.4: Ongoing standardized education focused on compassion fatigue, burn-out, and self-care, beginning at orientation to reduce staff stress, anxiety, and secondary post-traumatic stress disorder (PTSD) to maintain high-quality, ongoing support to families with babies in the intensive care unit should be provided.
Competency 3.5: A designated person with the psychological expertise to conduct education programs, as well as individual and group therapeutic consultation, should be identified to assess, plan, and implement a process to reduce staff and family stress, anxiety, and secondary post-traumatic stress disorder (PTSD), and promote self-care.
Competency 3.6: The unit’s operational budget expense and revenue, productivity, provider payment, insurance payment, and contractual agreements for improvement opportunities will be monitored to evaluate the value of IFCDC relative to the unit/organization vision, mission, practice, and outcomes.
Competency 3.7: Workforce scope of practice, competence, caseload, workload equity, worked hours, outcome, and safety occurrences to assess patterns and/or barriers that lead to the identification of improvement opportunities should be monitored.
Competency 3.8: Evidence-based improvement findings and recommendations shall be gathered, analyzed, and disseminated to unit, organization, community partners, and national collaborators through knowledge sharing/transfer and outcome transparency.
Competency 3.9: Health disparities and social determinants within the neonatal population should be recognized, monitored and improved through systematic data collection and education to address disparities and social determinants.
Evidence-based rationale:
Complex intensive care delivery systems should determine the relationship(s) between stakeholders, processes, and products, that influence the safe care provided to babies; and quantify the comparative value (including cost) of the influence. Historically, resources tend to be committed to care with insufficient evidence to support the value over time. Further, the non-utilization and/or withdrawal of resources may occur without regard to value, rationale, cost, or wellbeing. Because the wellbeing of staff directly affects the wellbeing of babies and parents, it is important to continuously evaluate performance, and provide education and training for intensive care staff, that adequately equips them with effective communication skills, self-care and coping strategies needed for the inherently high stress work of caring for premature and sick babies and families who are often in crisis. Health team members, preferably in-house, and families should invest in a culture of awareness and collaborative interaction within the system to provide value-added resources, evidence-based care initiatives, and continuous outcome evaluation (6, 12, 18, 19, 32-49)
Standard 4, Systems Thinking: The intensive care unit practice and outcomes will provide evidence that demonstrates the continuous monitoring of information relative to IFCDC practice.
Competency 4.1: Improvement initiatives and resulting neonatal health outcomes shall be monitored, evaluated, and communicated.
Competency 4.2: Health outcomes should be monitored using a standardized neonatal database.
Competency 4.3: Unit organizational outcomes should be compared with self, local, state, national, and international outcomes and population health goals, e.g. Healthy People 2020, community and state databases, Centers for Disease Control & Prevention Data and Statistics, March of Dimes Peristats.
Competency 4.4: Neonatal health and social determinants should be assessed and monitored for improvement opportunities.
Competency 4.5: A designated person with the appropriate qualifications to extract, program, manage and report data should be identified and accessed.
Competency 4.6: New knowledge, limitations, and value-added recommendations for implementation to improve IFCDC practice by the team shall be disseminated.
Evidence-based rationale:
The care provided to/with babies and their families is complex, and often long-term. The environmental, physical, social, behavioral, and pharmacologic aspects of care interact in a complex fashion so that it is difficult to determine the direct influence of one event, behavior, and/or therapy on another. Outcomes are likely the result of multiple factors. Consequently, all identifiable elements of the system should be monitored so that the data can be translated into meaningful information about the system. The interaction of data points, and the ensuing patterns that are evident over time, guide the interpretation of data for further study and evidence-based improvement. Potentially better practices can be identified from data interpretation to enhance decision-making and operational practice. Comparing evidence-based practice, process, and data among similar neonatal ICUs, provides a broader base from which to evaluate the value of the practice and the interpretation for meaningful change (2, 12, 18, 50-58)
Standard 5, Systems Thinking: The interprofessional collaborative practice team shall be transparent regarding the access and use of medical equipment, devices, and products; medications and vaccines, and technologies related to the IFCDC care in in-patient setting, home, and the community.
Competency 5.1: Evidence, short-term and long-term, for effective use with the baby to improve neurodevelopmental outcome shall be evaluated.
Competency 5.2: Professionals and parents shall be educated at the appropriate level of understanding in the use of devices, products, medications, vaccines, and technology, and implication for outcomes.
Competency 5.3: IFCDC practice, and the use of clinical devices and products, shall be standardized so that the team members, including the family, can become expert.
Competency 5.4: Use of equipment and products, activity at the point of service, and safety/recall notices shall be monitored.
Competency 5.5: Methods to evaluate the value of the equipment, device, product, medication and/or vaccine, and technologies for the baby, short- and long- term should be developed, implemented, and discussed among parents and staff.
Competency 5.6: Evidence learned through the implementation and evaluation process of equipment, device, product, medication and/or vaccine, and technologies for the baby, short- and long- term will be disseminated.
Evidence-based rationale:
Unit leaders, professionals, parents and families are accountable to be informed about nuances in equipment, devices, products, medications and vaccines, and technologies relative to the continuous care and monitoring of the baby. The evidence-based application to practice and care of each item should be evaluated as to relevance to neonatal outcome. Value should be weighed by comparing current therapy versus the new therapy, the initial cost of the item and the recuperation of expenditure through a patient charge over the period of time that the item is used, and the potential impact to outcome. Accessibility to new technology should be determined. The implementation of new equipment, devices, products, medications and vaccines, and technologies should be reviewed with all involved professionals and applicable service department representatives for a safety assessment, and education/training in the use. A trial may be warranted. Documentation and evaluation of the use of the item should be conducted. Transparency is important to the process of standardization, by disseminating the evaluation results of use and application, and identifying the implication to practice and outcome. (18, 19, 56-58)
Standard 6, Systems Thinking: The interprofessional collaborative team should provide IFCDC through transition to home and continuing care for the baby and family to support the optimal physiologic and psychosocial health needs of the baby and family.
Competency 6.1: Families should be encouraged to openly communicate and connect with other families who have lived the experience of in-hospital care, transition to home, and integration into the community.
Competency 6.2: Procedures that engage the family in assessing the readiness of themselves and the baby for transition to the home environment should be developed, implemented, and evaluated.
Competency 6.3: Multiple methods and tools, including simulation, to transfer information, education and training to families in order for them to demonstrate their ability to manage the care of the baby in a safe manner both in the hospital and at home, and to identify potential risk, should be utilized.
Competency 6.4: Assessment with the family of their confidence level, for managing the baby in the home and community environment, should be implemented.
Competency 6.5: Identification and assistance in the arrangement of resources post-discharge, including clinics, agencies, community programs, to support the growth and optimal function of the baby in the home and community environment should be available.
Competency 6.6: The IFCDC team will engage the family in arranging continuing follow-up care with health and wellbeing professionals, early intervention, and/or specialty team for post-discharge follow up.
Competency 6.7: Assessment of the practicality of the integrated electronic health information and data across service areas to support timely physical and psychosocial care and wellbeing of the baby and family should be implemented.
Competency 6.8: The IFCDC team and ICU system should identify, monitor and utilize standardized outcome indicators across the continuum of care to enhance long-term health outcomes.
Competency 6.9: Both in-hospital and appropriate follow up services should strategize improvement opportunities for continuity in education, care, system service delivery, policy, fiscal management, supplies, and equipment, across inpatient, outpatient, and community services.
Competency 6.10: Improvement initiatives involving in-patient, out-patient, and agency team members and families who have had infants in the ICU should be implemented and monitored.
Competency 6.11: The transfer of improvement findings and the lived experience of families should be provided in a transparent manner.
Competency 6.12: Efforts to sustain fiscally-sound, value-based, and safe, continuing improvement of care at home should be explored.
Evidence-based rationale:
Babies with complex needs, and their families, is a small, expensive, and underserved population whose health outcomes are inadequately monitored and reported through their lifespan. The current medically-based model does not adequately serve individuals and families with their continuum of growth, cognitive, physical, and psychosocial needs. Hand-offs from medical team to medical team over the lifespan, interrupt health progress, and confuse, sometimes ignore, family members and caregivers. Further, the limited whole-person longitudinal data of the population creates a knowledge deficit for the health professionals managing needs in the home and community during the lifespan. Re-design of the model of continuing care following the transition to home would facilitate a system of interprofessional collaboration, to empower the family, to function independently, communicate openly, disseminate learning, manage change, facilitate collective action, resolve conflict, and make decisions jointly while prioritizing the needs of the family. The interprofessional collaborative team(s), within and outside of the organizational system, is challenged with the responsibility to guide families through the multiple service levels of the health continuum and cultural environment, manage needs, and strengthen the optimum health outcome of the baby and the family. (12, 39, 59-75)