IFCDC- Recommendations for Best Practice for Positioning and Touch
“Imagine…holding your daughter’s hand, and its entire width fits across the tip of your finger.”*
These committee members had primary responsibility for this section:
Jan McElroy, PhD, PT, PCS, C/NDT
Jane Sweeney, PhD, PT, PCS, FAPTA
Questions to consider when starting your process Positioning And Touch For The Newborn
Check sheet to assess this area before and after intervention.
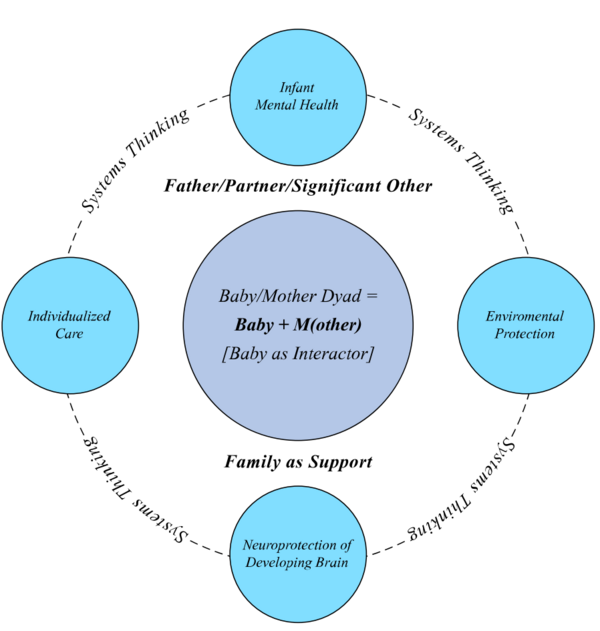
Successful change only happens in relation to the system. To review systems concepts check this section
Standard 1, Positioning and Touch: Babies in intensive care settings shall be positioned to support musculoskeletal, physiological, and behavioral stability.
Competency 1.0: Body position shall be individualized and monitored for head, trunk and extremity alignment and movement.
Competency 1.1.1: Supine position should include head and trunk alignment in neutral (not flexed or extended) with semi-flexed extremity posture and use of nested containment with positioning materials.
Competency 1.1.2: Midline head position in supine and side-lying should be considered to minimize potential risk of germinal matrix- intraventricular hemorrhage during the first 3 days after birth in babies born at or less than 32 weeks of gestation.
Competency 1.1.3: Positional support should promote and not restrict spontaneous extremity movement.
Competency 1.1.4: To address and model sleep safety for the home environment, prior to discharge, babies previously positioned therapeutically in varied sleep positions and who are medically stable, should be transitioned to the supine position on a flat, firm bed surface without positioning aids or loose bedding materials.
Competency 1.1.5: Prone position may be used with a vertical positioning roll (from clavicle to pubis) to facilitate extremity flexion. Continuous cardio-respiratory and oxygen saturation monitoring for preterm babies positioned in prone. Mechanically ventilated preterm babies may be judiciously transitioned to prone to improve oxygenation.
Competency 1.1.6: Side-lying position may be used on an individualized basis for spontaneously breathing preterm babies.
Competency 1.2.0: Individualized application of a swaddling blanket may be used to support body alignment and allow lower extremity movement in supine, prone, and side-lying positions.
Competency 1.2.1: Preparation for body alignment with swaddling should include placing hands toward the mouth or face, moving legs into a semi-flexed, abducted position, and keeping neck and trunk alignment neutral without flexion or extension.
Competency 1.2.2: Space for spontaneous kicking shall be created inside the swaddled containment to reduce the risk of hip dysplasia from excessive hip adduction and extension posture.
Competency 1.2.3: Swaddling during weighing, bathing, and heel lance may be used to modulate physiological and behavioral stress during routine care.
Competency 1.2.4: Swaddling may be used as a non-pharmacological comfort strategy for babies with behavioral irritability or neonatal abstinence syndrome.
Standard 2, Positioning and Touch: Collaborative efforts among parents and ICU interprofessionals shall support optimal cranial shaping and prevent torticollis and skull deformity.
Competency 2.1: Positioning for symmetry and neutral alignment shall be implemented, monitored, and documented to promote cranial shaping, and prevent muscular torticollis.
Competency 2.2: Daily variation of head positions (lateral and midline) shall be monitored, and repositioning the crib for head turn variation shall be considered within the assigned bed space.
Competency 2.2: Neonatal therapy for asymmetrical head position preference and skull deformation shall be implemented with pediatric therapy follow up after transition to home.
Standard 3, Positioning and Touch: Body position shall be used as an ICU intervention for infants with gastrointestinal symptoms.
Competency 3.1: Babies with gastroesophageal reflux should be placed in prone (optimal) or left side after feeding.
Competency 3.2: Babies with gastric residuals should be placed in prone or right side after feeding.
Competency 3.3: Bed elevation (30 degrees) with right side-lying position may be used to decrease aspiration of gastric residuals.
Competency 3.4: Bed elevation (14-15 degrees) may be used to reduce tracheal aspiration in ventilated babies.
Evidence-based rationale:
Varied body positions are indicated for postural alignment, extremity movement, and physiological stability with repositioning at 3 to 4 hour intervals. (1) Supine positioning within a containment “nest” formed by blanket roll boundaries, or positioning aids, promotes semi-flexed posture, reduces spine hyperextension, and facilitates midline movement. (1-4) Prone positioning with a vertical positioning roll under the thorax improves hip flexion posture and scapular alignment. (5) Improved oxygenation was found only in the prone position in preterm infants on mechanical ventilation. (6) Long, deep sleep periods associated with the prone position may increase vulnerability to sudden infant death syndrome, indicating the need for physiological monitoring of infants in the prone sleep position in the NICU. (7) Side-lying sleep position was not associated with adverse cardiopulmonary effects (apnea, bradycardia, or oxygen desaturation) in spontaneously breathing preterm infants at <28 weeks postmenstrual age (PMA) and <1000 grams birth weight. (8) Despite limited rigor of evidence analyzed by a Cochrane Neonatal Review Group, Romantsik et al. (9) maintains that midline head position in supine and side-lying may be prudent for minimizing germinal matrix-intraventricular hemorrhage during the first 3 days of life in babies born at or under 32 weeks of gestation until further research supports, or refutes, midline head positioning. Transition to the supine sleep position on a flat, firm surface without positioning aids prior to discharge was recommended by the American Academy of Pediatrics (AAP) to model a safe sleep environment to 12 months of age. (10)
Swaddled babies had improved neuromuscular development and motor organization, less physiological distress, longer sleep duration, and improved behavioral self-regulation. (11) Body swaddling within a containment “nest” resulted in recovery of autonomic and motor stability within 5 minutes of weighting and bathing infants at 32 to 35 weeks PMA. (12) Crying and temperature loss decreased during swaddled immersion bathing compared to unswaddled bathing. (13, 14) Increased physiological and behavioral organization occurred during swaddled weighing. (15) Decreased pain response occurred 3 and 7 minutes post-heel stick procedure in swaddled versus containment only position. (16) Swaddling should be considered a non-pharmacological standard in the care of babies with neonatal abstinence syndrome (NAS) (17). Tight swaddling, with restriction of kicking movement, and hip mobility, increases vulnerability for developmental dysplasia of the hip. (18)
Positional skull deformation related to NICU body positioning was detected in preterm infants at 32 to 34 weeks PMA and at term equivalent age. (19, 20) Physical therapy management of positional plagiocephaly was superior to repositioning education and repositioning devices. (21) Timely physical therapy referral and intervention are indicated to manage the clinical pattern of plagiocephaly and asymmetrical motor performance in preterm infants (22). Severe deformational plagiocephaly was significantly lower in babies receiving intermittent outpatient physical therapy intervention at 7 weeks to 12 months of age. (23)
Body position influences gastric emptying and reflux. Babies placed in prone and left side-lying positions had decreased reflux. (24) Gastric residual was reduced in the prone and right side-lying position (25) with immediate prone positioning recommended in the first 30 minutes after feeding. (26) To manage combined gastric residual and gastroesophageal reflux, recommendations include positioning babies in prone or right side lying position with repositioning based on individualized behavioral responses. (26, 27) Bed elevation at 14 to 15 degrees resulted in decreased tracheal pepsin aspirate in ventilated babies. (26-28) Bed elevation of 30 degrees combined with right side-lying position for 6 hours were associated with decreased pepsin aspirate compared to elevated, supine position in ventilated babies. (29)
Standard 4, Positioning and Touch: Babies in ICU settings shall experience human touch by family and caregivers.
Competency 4.1: A parent should be invited to participate with the primary caregiver to provide support to the baby during potentially stressful caregiving and medical procedures. When parents are unavailable, a second caregiver should support the infant.
Competency 4.2: The need for personnel staffing for intermittent procedural assistance in touch and comfort support is essential should be accommodated.
Competency 4.3: Individualized gentle touch (without stroking or passive joint movement) to the head, chest, back, and/or under feet shall be provided when the baby is in an awakened or distressed state and not during quiet sleeping.
Competency 4.4: To avoid overstimulation, individualized frequency and duration of supplemental, gentle touch shall be determined by evaluating the baby’s behavioral and physiological parameters before, during, and after the touch interaction.
Competency 4.5: Supplemental gentle touch shall be used judiciously with diligent monitoring for babies with low gestational age and high acuity to insure stability and avoid behavioral agitation, oxygen desaturation, and bradycardia.
Competency 4.6: Stabilizing hand support and slow movement transitions during routine caregiving tasks shall be used for infants with fragile bones, infusion lines and tubes, and ventilator or respiratory equipment.
Evidence-based rationale:
Gentle touch was an effective assist with pain management in the ICU during selected medical procedures. (30-33) Decreased motor stress and increased self-regulatory behaviors during endotracheal suction procedures were found when 4 handed-care was provided by 2 providers. (34) Decreased heart rate and increased REM sleep were calming effects of touch. (35) Rather than using a timed routine for therapeutic application of touch, continuous evaluation and modification of touch should be synchronized with each baby’s physiological and behavioral patterns (36). Fragile babies with high morbidity scores and low gestational age (29.4 weeks) were vulnerable (bradycardia and desaturation) to overstimulation with gentle human touch. (35)
*Acknowledgement of Diane Maroney for consenting to our use of the concept of “imagine…” statements written by parents/families who have experienced intensive care; and to our parents for their thoughts.